
degree of osteochondrosis
- The initial stage is characterized by lesions within the disc. It loses water, leading to degenerative changes, loss of disc height, and rupture of the fibrous capsule. Generally speaking, there are no signs at this stage. Diagnosis can only be made with an MRI of the spine. This is the most favorable stage to start treatment, since in this case the damaged disc can be completely restored, which will not be possible in the future.
- Second-degree osteochondrosis is characterized by worsening of disc damage. Their height decreases significantly, causing the spinal muscles and ligaments to sag. All of these can lead to instability of the damaged portion of the spine, increased mobility of the vertebrae, shifting and sliding of the vertebrae relative to each other and the spinal axis. Usually, at this stage, the first symptoms of the disease appear in the form of pain and other symptoms specific to cervical spine pathology.
- In the third stage, disc herniation and herniation occur. The symptoms of the disease are fully represented.
- The fourth stage is the final stage. In this case, osteophytes and spinal deformity develop. The body attempts to somehow stabilize the damaged portion of the spine, which is why osteophytes, ossification of ligaments, and other processes that lead to vertebral stabilization occur, but unfortunately, this process is accompanied by vertebral subluxation and various types and degrees ofVertebral subluxation. Spinal deformity.

Nature of symptoms of cervical osteochondrosis
- Direct compression of the spinal cord as it runs in the spinal canal. It should be noted that this rarely occurs in advanced degenerative processes and their complications. Huge intervertebral hernia extends directly into the spinal canal cavity, which can cause compression of spinal cord nerve tissue; spinal canal stenosis (narrowing) due to degenerative changes; dislocation, subluxation, and fracture of damaged vertebrae.
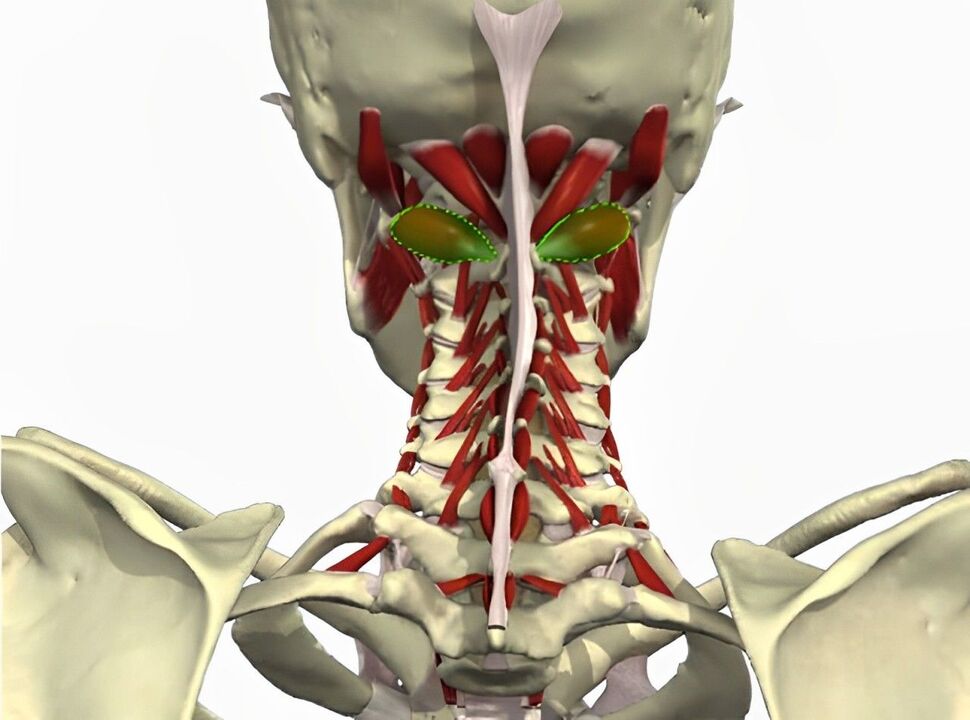
- Negatively affects the structure of the cervical peripheral nervous system (spinal roots and nerve fibers). They may become compressed between adjacent vertebrae or herniated bulges and may become inflamed and inflamed. All of these can lead to many serious symptoms. This is the most common set of symptoms of cervical osteochondrosis.
- Negatively affects the blood vessels that pass near the damaged area of the spine. In particular, a very important arterial blood vessel is of clinical significance - the vertebral artery, which passes through the opening of the transverse process of the cervical vertebrae into the cranial cavity and supplies blood to the posterior third of the brain and cerebellum.
Symptoms associated with spinal cord injury
Symptoms related to nerve damage
pain syndrome

radiculopathy syndrome
Occipital neuralgia
cardiac syndrome

Symptoms associated with vertebral artery injury
- Diffuse or throbbing headache in the back of the head, temples, and parietal areas;
- Dizziness;
- nausea and vomiting;
- visual impairment;
- Tinnitus, decreased hearing acuity;
- Impaired coordination and balance;
- Having a fall attack (falling suddenly without losing consciousness due to a sudden turn of the head);
- Memory loss, decreased performance, and difficulty concentrating.












































